Everything you need to know about herpes simplex (and why it’s no big deal)
What is herpes simplex?
Herpes simplex is a viral infection caused by the herpes simplex virus. It typically presents as painful blisters and sores on and around skin of the mouth, genitals and/or anus, though it can appear on other parts of the body. There are two types of herpes simplex virus (HSV): HSV-1, which is typically associated with cold sores around the mouth, and HSV-2, which is usually associated with cold sores in the genital area. And I’ve deliberately used the word cold sores for the genital kind because it’s essentially the same thing.
The way people view the oral kind is vastly different to the way those same people view the genital kind, and perhaps that’s to do with the fact it’s on the genitals. And we’re all a bit funny when it comes to anything affecting our genitals, right? The reality however, is they are very similar infections. So similar that you cannot tell which viral strain, 1 or 2, has caused a given infection by symptoms alone. A blood test or swab will be required. That’s because not only are the symptoms identical, but HSV1 can and does cause genital herpes and HSV2 can cause oral herpes; albeit HSV2 rarely causes an oral infection. In developed nations up-to 50% of genital herpes are caused by HSV1, the “oral” herpes virus. More on this later.
How common is herpes simplex infections?
It’s important to understand just how ubiquitous herpes simplex infections are. Whilst prevalence varies country to country we can paint with very broad strokes and say in most developed countries, HSV1 infects somewhere between 50 – 90% of the population, whilst HSV2 infects between 10 – 25%. In less developed countries HSV1 infects nearer to 90% of the population and HSV2 prevalence can be as high as 60%. Before you freak out, somewhere between 66% and 90% of those infected are completely unaware, and that’s really important to remember because for most people being infected with one of the herpes simplex viruses does not impact their lives.
For the minority of those infected that do get symptoms, the majority of them will experience only mild symptoms, and that’s also important to remember. It’s an occasional nuisance. Those images you’ve probably seen over the internet or during sex education are a bad outbreak of blisters, but most of the time it doesn’t look like that. Herpes can present as an occasional mild itching, or perhaps a small red rash without blisters. Other times it can present with blisters, but perhaps only a couple, perhaps only a single blister. It’s this variability in symptoms that can make diagnosis difficult. Particularly for those with such mild symptoms, they are often attributed to something else and herpes isn’t even considered as the cause. The physical aspects of having herpes for most people is a non-issue, although there is a sub-set of patients who do get painful and frequent episodes – and that’s why a cure to rid the body of the virus would be great!.
Can you be infected with herpes and not know it? Is it possible to have herpes for years and never know?
Assuming you’ve never had an outbreak the only way to know whether or not you’ve been infected is by testing. And the reality is most of us never have never been tested, and health authorities recommend against screening for HSV without symptoms.
It’s not something we routinely check for, not even during a full STD check up. And when I tell you it’s not routinely screened for, I mean when you go the local sexual health clinic and get a full panel of STD tests, a test for herpes isn’t included. That includes the NHS service and most private clinics too.
Even on letsgetchecked.com, the most expensive STD test kit they sell (Complete 11 currently sold for £199) only includes a urine test for HSV, a test that can only detect HSV during an outbreak. That means if you have been infected with herpes simplex and are one of the majority that experience no symptoms, the test is likely to report back negative. Even for those that do experience occasional symptoms, the test will be likely return a negative result if at the time of taking it they are symptom free.
There is a blood test that can detect if you have been infected but you may have to wait up to 6 months before it shows up on the test, because for some people it can take that long for the body to produce the type of antibody the test is looking for. This means if you were infected today, it may take 6 months for that test to return a positive result. The test doesn’t look for the virus but looks for the antibody the body produces in response to the infection. The test is called a HSV IgG test because it’s detecting the presence of the IgG antibody.
How does HSV spread?
HSV is primarily transmitted through direct skin-to-skin contact with an infected individual. It’s a little more complicated than that because transmission can only occur when the virus is active on the skins surface, and thanks to a phenomenon called silent shedding, we can never be certain when that is. Obviously when someone is experiencing an outbreak of blisters we can be certain the virus is active, and it is at that point they are most contagious. Similarly whenever an infected individual feels an itchy sensation, that too can indicate the virus is active. Other times, the virus will be active but the patient will experience no symptoms whatsoever, this is called silent shedding and it is said that the majority of herpes transmissions occur during episodes of silent shedding. In fact a lot of people only find out they have herpes after they transmit it to a partner who then develops symptoms.
Remember how earlier we said most people, up to 90% of people, experience no symptoms? Well, that doesn’t mean they don’t shed the virus, and therefore they can still infect others, who have a 90% chance of also not experiencing symptoms but who too can spread the infection. You can probably start to see why so many people are infected as it tends to spread unchecked.
The virus can be present in the saliva, genital secretions, or lesions of an infected individual and it can spread through activities like kissing and sexual intercourse (including oral). It cannot be transmitted through inanimate objects such as a towel or toilet seat, as the virus dies very quickly outside the body.
Why are herpes simplex infections permanent? Why is there not cure for herpes?
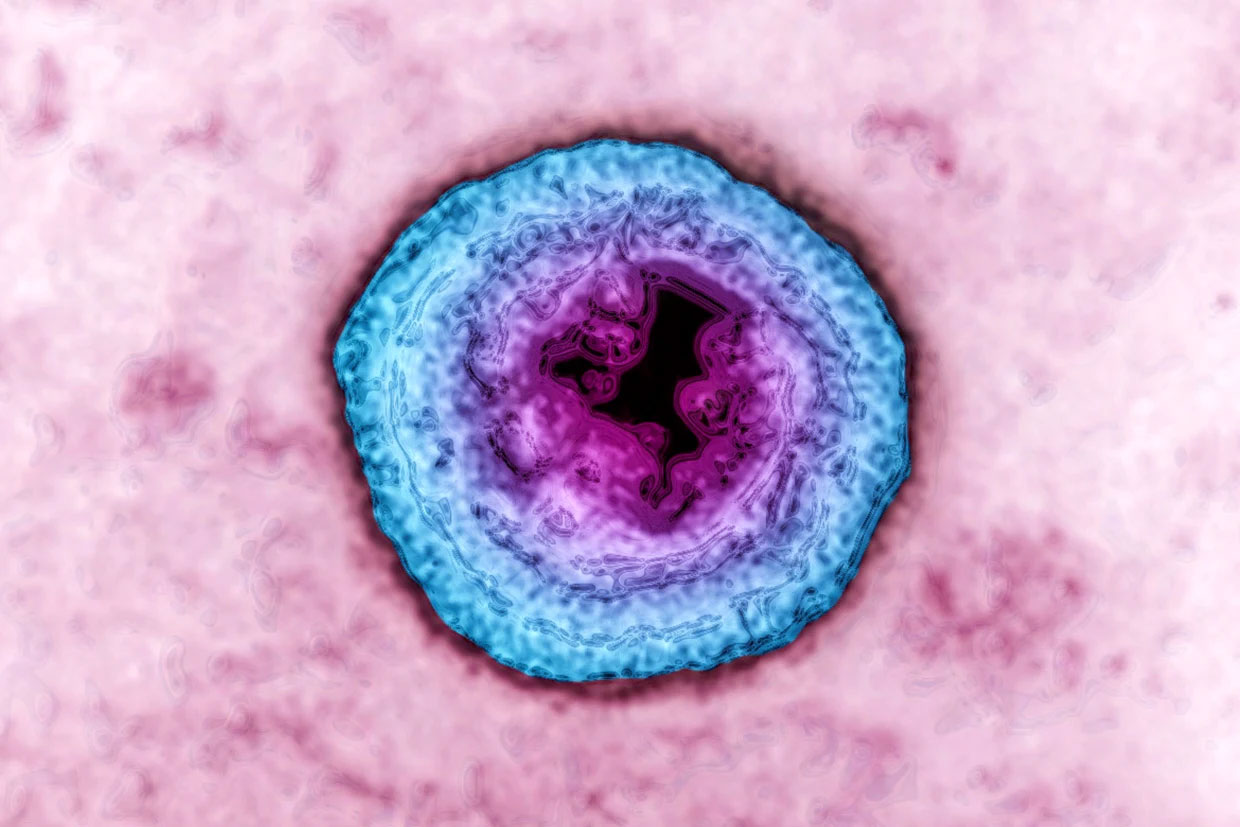
When HSV comes into contact with the skin, it targets and infects epithelial cells, a fancy word for skin cells, and the virus is particularly good at infecting mucous membranes. Mucus membranes are the wet parts of our bodies that are exposed to the outside world, like the mouth, vagina or pee hole. Once inside HSV starts to replicate and like a homing missile, HSV seeks nerve endings at the site of the infection. The virus travels along nerve fibres to the nerve cell bodies, called ganglia, and it is here in the ganglia that HSV hides away from the body’s immune system and establishes a ‘latent’ infection.
Given enough time our bodies learn to identify HSV infected cells and has no problem clearing the virus from the skin. We know that to be true because whilst medication can reduce the duration and severity of an outbreak, our bodies can fight it off even without pharmaceutical assistance.
However, and this is a big however. Our bodies cannot fight the virus when the virus hides away in the ganglia. For this article I won’t get into in the reasons why that is the case but note the key takeaway, once the nerve ganglia have been infected, the infection is permanent.
What is latency?
You can think of latency as sleep. When the herpes simplex virus is latent, it is asleep, or dormant. Whilst asleep, or dormant, the virus is not active. It is not replicating; it has very limited activity and it cannot be transmitted to another person.
HSV infections switch between actively replicating and sleeping, or latency. It is for this reason persons infected with the virus are not constantly experiencing symptoms but may occasionally. Even when the virus does become active our bodies are pretty quick to react and force the virus back into its sleeping state. Other times HSV gets the upper hand and causes an active outbreak or sheds at the surface of our skin before being beaten back down by our immune system.
How to prevent infection from herpes simplex viruses?
Prevention is indeed important. To reduce the risk of HSV transmission, it’s advisable to avoid direct contact with active lesions or bodily fluids of an infected person. For the genital kind, consistent and correct use of barrier methods, such as condoms or dental dams during sexual activity can help minimize the risk of infection but cannot eliminate it. It’s important to note that even when no visible symptoms are present, HSV can still be transmitted, and as mentioned earlier, this is likely the most common time HSV is transmitted.
The reality is that unless you decide to never interact with another human being ever again, HSV is pretty hard to avoid. Particularly the oral infection. You risk it anytime you kiss anyone, and you risk it whenever you have sex.
Condoms can help protect against the genital kind but they’re not 100% effective as they don’t completely cover the entire genital region, and sex involves a lot of skin-to-skin contact. The base of the penis is exposed, the balls, the thighs, the vulva and so on. All skin that HSV can infect. It is estimated that condoms only reduce the risk for men by around 30-50% percent but may reduce the risk to women by up to 96%. So wrap up.
That being said if we assume a couple has unprotected sex twice a week, and one of them has HSV, the risk of the man being infected by the women is estimated to be 4% per year, and the risk for the women is around 10% per year. Women are just more likely to be infected in the first place, and that comes down to the mucus membrane thing we spoke of earlier. A vagina has more mucus membranes than a penis, and so infection is more likely, not just for HSV but all STI’s.
Suppressive therapy can also help reduce the risk of transmitting HSV to a partner. This involves taking medication on a daily basis to decrease shedding and the frequency and severity of outbreaks. It is important for both partners to communicate openly about their sexual health, get tested regularly, and take necessary precautions. A large study estimates that suppressive therapy can reduce risk of transmission by 50%, although it’s not clear if this is in addition to the protection offered by condoms alone.
How to test for herpes simplex infection?
If you’ve never had symptoms and want to know, take an IgG blood test. This will be able to determine if you have been infected with herpes simplex and determine which strain too. That being said it is only 70% accurate for detecting HSV1 but 90% accurate for detecting HSV2. In other words 30% of those infected with HSV1 will receive a false negative result, and 10% of those infected with HSV2 will receive a false negative result. False positives happen too.
If you have symptoms, blisters in particular, you should have the blisters swabbed. Swabs provide testing in one of two methods, culture and PCR testing. Culture testing is used to grow the virus from a sample taken from the blisters. PCR, or polymerase chain reaction, testing detects the genetic material of HSV and can provide results within a matter of hours rather than days like culture testing. Both tests are able to determine which strain of HSV (1 or 2) have caused the the infection. Of the two, PCR testing is preferred. It’s more reliable, sensitive and as mentioned, quicker to get the results. A positive result from PCR testing can be considered 100% accurate i.e. the chance of a false positive is almost non-existent.
If you’re experiencing your very first outbreak, do both the PCR swab and IgG blood test. This will give you an indication whether or not you’ve been recently infected. See the table below to understand what the results indicate:
| IgG Negative | IgG Positive | |
|---|---|---|
| PCR Swab Negative | Not infected | Blister is not caused by HSV (or poor sample) however, previous infection detected (IgG) |
| PCR Swab Positive | Recently infected | Infected, but the infection is not new |
There is another blood test called the IgM but it is wildly inaccurate and most health authorities has discredited it as a diagnostic tool, including the CDC.
Finally, there is another test, the gold standard. The university of Washington owns the exclusive rights to test and they are the only people that can do it. Consequently, it’s a challenge to get it done outside USA. It’s called the ‘Western Blot’ if you’re interested.
Shedding: How often does herpes simplex shed?
HSV is not always active. It fluctuates between an active state and a dormant state. Depending on the virus (1 or 2) and the location of the infection, the viral activity can vary.
By taking regular swabs and testing using PCR, we can estimate the activity of the virus based on what percent of swabs detect the virus. As the PCR testing is highly sensitive, it will detect virus even when the patient is experiencing no symptoms.
The table below summarises how often HSV is estimated to shed, although the reality is that it is highly variable between individuals. People who are infected and experience zero symptoms (asymptomatic) are estimated to shed half the amount as symptomatic individuals.
| Oral Infection | Genital Infection | |
|---|---|---|
| HSV1 | 30% | 10% |
| HSV2 | Almost never | 30% |
Shedding also tends to be higher in the first year of infection and then declines as our bodies learn to fight the infection better. That being said, one study showed that after 10 years, patients with a genital HSV2 infection still shed over 10% of the time. More studies are needed to be done in this area.
How often are outbreaks experienced?
Some people think, if you have genital herpes you’re covered in blisters 24/7. That’s not the case. At the end of the day it can be an added nuisance but, if you get it, you will be okay. Not much will change, you’re life isn’t over, your sex life isn’t over. It’s crazy that I need to write that but it’s too common for patients to freak out when they receive a herpes diagnosis, less so with oral herpes, but certainly with the genital kind.
The table below show the number of outbreaks that can typically be expected in the first couple years after an infection with HSV1 and HSV2, either orally or genitally
| Oral | Genital | |
|---|---|---|
| HSV1 | 1-4 | 1 |
| HSV2 | Rare | 1-4 |
But as we’ve already covered, this is highly variable. HSV1 tends to be more active orally than genitally, whilst HSV2 is more active below the belt than above. This means that genital HSV1 infections typically only manifest in symptoms once a year and for many, after the first year only once every few years, possibly never again for some.
In contrast genital HSV2 may manifest itself with 4 outbreaks a year in the first couple years, but this is highly variable. Some people will experience only a single outbreak ever, whilst others may get 6 outbreaks a year. The same is true for oral HSV1 infections, some people rarely get an outbreak, whilst others get them monthly.
There no predicting how many outbreaks an individual will experience once infected, or if they even will experience any outbreaks. Remember the majority of those infected do not know they are infected because they are asymptomatic.
What we can say with a high degree of certainty is the first outbreak tends to be the worst as the immune system is not prepared to deal with the infection. The first outbreak can take up to 3 weeks to heal regardless of strain or location. Subsequent outbreaks are milder because the body learns to recognise the virus and does a good job fighting it. Overtime the number of outbreaks reduce and they tend to last only 3- 7 days.
All that being said, with treatment the number of outbreaks can be reduced to zero for many people and certainly at least a 70% reduction for most. We cover treatments a little further down.
Emotional distress and stigma
I’d argue that the emotional distress from a herpes diagnosis, particularly the genital kind, is worse than the physical symptoms. A minority contemplating suicide. That is bonkers. Most of that is driven by the social stigma of having herpes, which is driven by false information. At end of the day, when push comes to shove, it’s a rash. A contiguous rash which is the rubbish part, but for the most part it’s just a rash. In fact the number one concern for those with the infection is passing it on to others, not the physical aspect of having the infection.
Treatments for HSV infection
While there is no cure for herpes simplex, there are a variety of treatments available to manage symptoms and reduce the frequency and severity of outbreaks. But that’s the thing, most people have no symptoms despite being infected. Treatment however can also be used to reduce the risk of transmission by 50% and being as that is the number on concern for those infected, it can help with the mental aspect too.
Current treatments for herpes simplex
Antiviral medications are the most common and effective treatment for herpes simplex. These medications work by blocking the replication of the virus, which can help to reduce the duration and severity of outbreaks. There are several antiviral medications available but they are all based on acyclovir, a medication that came out in the 1970’s:
- Acyclovir is a classic antiviral medication that is available in various forms, including oral tablets, topical creams, and intravenous injections. It is the most commonly used medication for the treatment of herpes simplex and can be used for both acute and chronic infections.
- Valacyclovir is a prodrug of acyclovir, that means it is converted to acyclovir in the body. The advantage of valaciclovir is that more of it is absorbed when compared to acyclovir, and that means less frequent dosing is possible. It is available in oral tablet form.
- Famciclovir is another antiviral medication that is used for the treatment of herpes simplex. It is available in oral tablet form and can be used for both acute and chronic infections.
The mechanism of action of acyclovir, valacyclovir and famciclovir is that they inhibit the replication of viral DNA by acting as a chain terminator. This means they prevent the virus from making copies of itself, thereby slowing down the rate at which it can replicate and spread. Due to the mechanism of activity, these antivirals only work when the virus is actively replicating, and not the latent infection. That’s why they can’t reduce transmission by 100%.
In addition to antiviral medications, there are several other treatments available for the management of herpes simplex. These include:
- Analgesics (pain killer medication)
- Numbing creams
- Lemon balm / Melissa
- Tea tree oil
- Lysine
Over-the-counter pain relievers, such as paracetamol (acetaminophen) or ibuprofen, can be used to relieve the pain associated with an outbreak of blisters. In addition, some people will experience a fever when first infected and analgesics can help with this too. Additionally, numbing creams containing lidocaine can be applied to the affected area to reduce pain and discomfort.
Some people may find relief from topical herbal remedies such as lemon balm or tea tree oil, which have been traditionally used for their antiviral properties.
Finally, supplementing with the amino acid Lysine has been shown to help reduce the frequency and duration of herpes simplex outbreaks. Lysine works by blocking the action of another amino acid, Arginine, which is necessary for the virus to replicate. By limiting Arginine levels in the body, Lysine can help suppress viral replication and prevent outbreaks. From my research into peer reviewed studies, the evidence for is Lysine is somewhat muddy. That being said many swear by it. For those interested in trying it, the recommended dose is between 500mg and 3000mg per day.
It is important to note that these treatments may not work for everyone and should be used under medical supervision.
Avoiding triggers
Aside from medication and topical treatments, there are steps that can be taken to avoid triggers that may cause herpes simplex outbreaks. These triggers vary from person to person but can include:
- Stress
- Fatigue
- Exposure to sun (UV) or wind
- Coffee
- Chocolate
- Hormonal changes
By identifying and avoiding these triggers, it is possible for some individuals to reduce the frequency and severity of their outbreaks.
Potential future treatments for herpes simplex (up-and-coming treatments)
Research into potential new treatments for herpes simplex is ongoing, with promising results in recent studies. While current treatments for herpes simplex are effective at managing symptoms and reducing the frequency of outbreaks, there is ongoing research into developing more effective treatments and a potential cure for the virus.
New treatment can broadly be classified into one of four categories: helicase-primase inhibitor (antiviral), immunotherapies, vaccines and gene editing.
Helicase-primase inhibitors
Helicase-primase inhibitors are a promising new class of antiviral that work by inhibiting the enzymes responsible for forming new viral DNA. By blocking this process, helicase-primase inhibitors can prevent the replication of the virus and potentially stop the spread of the infection.
Unlike our current set of antivirals (thymidine kinase inhibitors) that work only on actively replicating virus, helicase primase inhibitors have the potential to work on enzymes prior to any replication. This means they have the potential to not only treat active outbreaks, but also prevent future outbreaks and shedding. Used in combination with thymidine kinase inhibitors (acyclovir, valacyclovir and famciclovir) they may offer the one-two punch to keep herpes simplex viruses in their sleeping state, and thereby reducing or eliminating the risk of transmission.
Immunotherapies
Immunotherapies are another avenue of research for treating herpes simplex. These treatments aim to boost the immune system’s ability to fight off the virus and keep it in a latent state.
One promising immunotherapy is a drug called squaric acid dibutyl ester (SADBE). Results from a phase 2 study demonstrated that when applied topically, SADBE significantly extended the time to next herpes outbreak and reduced both the frequency and severity of outbreaks.
Vaccines
Vaccines come in two types:
- Therapeutic vaccines aim to help those already infected. The goal is to either reduce viral replication, or potentially eliminate it. If viral replication is eliminated this is known as a functional cure; the virus still infects the cells, but as it is not ever active, it essentially works as good as a cure.
- Prophylactic vaccines aim to stop the virus infecting the ganglia, and therefore stop it from becoming a permanent infection. Remember, as humans we have no problem fighting HSV. The main issue is eliminating HSV from the ganglia once infected, as these are privileged sites and therefore out of reach for our immune system.
Gene editing
Gene editing treatments are the most exiting development because they offer the potential for a cure, something that was previously thought of as not possible. Whilst there a few horses in the race, the leader of the pack is Keith Jerome with the Fred Hutch Cancer Research Centre.
They’ve shown that snipping the viral DNA in more than one spot significantly reduces the virus’s ability to repair it’s DNA . His team has developed a gene editing tool that can accurately cut the herpes simplex genome at two specific sites, effectively removing the entire viral DNA from the ganglia and potentially curing the infection.
HSV, pregnancy and the immunocompromised
Whilst throughout this article emphasis has been made on how little HSV effects those without immune deficiencies, it’s important to note that this virus can have far worse consequences for those who are immunocompromised. This is particularly true for pregnant women and their unborn children.
Those with a weakened immune system have a higher chance of being symptomatic, having more outbreaks, and more severe outbreaks. In addition, people with weakened immune systems are more susceptible to developing severe complications from HSV such as encephalitis (inflammation of the brain) or meningitis (inflammation of the lining of the brain and spinal cord); though these are still rare complications.
Pregnant women risk passing the infection to their baby which can be fatal. Thankfully even for those infected with genital HSV it’s very rare. Some healthcare systems recommend a caesarean if the mother is having a genital outbreak at time of delivery and most will recommend the mother uses suppressive therapy (acyclovir) in the third trimester to reduce the risk of transmission, and prevent an outbreak during delivery.
Conclusion
Herpes simplex is a common and often frustrating viral infection that can cause painful blisters and sores. While there is currently no cure for the virus, there are a variety of treatments available to manage symptoms and reduce the frequency of outbreaks. Antiviral medications are the most common and effective treatment for herpes simplex, but there are also other treatments available, such as topical creams and lifestyle modifications.
If you’ve recently been infected I recommend you watch this Adam Ruins Everything episode to help put yourself at ease
Last updated: OCT-2025